Translate this page to any language by choosing a language in the box below.
There are frequent news stories - and anecdotal reports - of the inaccuracy
of the COVID-19 tests. We all have a friend or relative who was tested
and it turned out to be false - either claiming they didn't have the virus when
they actually did (false negative) or the test says they do have the virus when
they didn't (false positive). 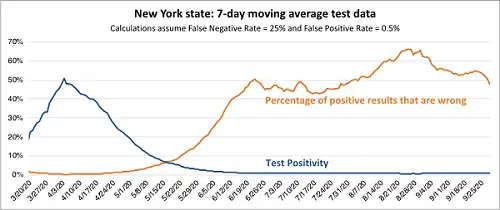
Harvard University says "The true accuracy of tests for COVID-19 is uncertain..Unfortunately, it' s not clear exactly how accurate any of these tests are. " False positives and false negatives can range from 20% to 70%. See an example graph of the PCR False Positives for NY State, from IDC University.
There are three types of tests;
| Molecular Test | Antigen Test | Antibody Test | Home tests | |
|---|---|---|---|---|
|
Also known as... |
Diagnostic test, viral test, molecular test, nucleic acid amplification test (NAAT), RT-PCR test, LAMP test |
Rapid diagnostic test (Some molecular tests are also rapid tests.) |
Serological test, serology, blood test, serology test |
The FDA recently granted EUA for a home molecular test that requires no prescription |
|
How the sample is taken... |
Nasal or throat swab (most tests) Saliva (a few tests) |
Nasal or throat swab |
Finger stick or blood draw |
Nasal or throat swab |
|
How long it takes to get results... |
Same day (some locations) or up to a week |
One hour or less |
Same day (many locations) or 1-3 days |
several days to a week |
|
Is another test needed... |
FDA claims, this test is typically highly accurate and usually does not need to be repeated, but Harvard University says: " The reported rate of false negatives is as low as 2% and as high as 37%. The false positive rate - that is, how often the test says you have the virus when you actually do not - should be close to zero. Most false-positive results are thought to be due to lab contamination or other problems with how the lab has performed the test, not limitations of the test itself.". |
Positive results are claimed to usually highly accurate but negative results may need to be confirmed with a molecular test. |
Sometimes a second antibody test is needed for accurate results. Isn't that great... |
|
|
What it shows... |
Diagnoses active coronavirus infection |
Diagnoses active coronavirus infection |
Shows if you've been infected by coronavirus in the past |
Diagnoses active coronavirus infection |
|
What it can't do... |
Show if you ever had COVID-19 or were infected with the coronavirus in the past |
Definitively rule out active coronavirus infection. Antigen tests are more likely to miss an active coronavirus infection compared to molecular tests. Your health care provider may order a molecular test if your antigen test shows a negative result but you have symptoms of COVID-19. |
Diagnose active coronavirus infection at the time of the test or show that you do not have COVID-19 |
Antigen tests are faster but have a high false negative rate: 40-50% and they may have an elevated false positive rate.
PCR tests have been found to miss positive cases (false negative) 30% of the time. We could find no reported facts about false positives. The Mayo Clinic says: "if sent to an outside lab. PCR tests are very accurate when properly performed by a health care professional, but the rapid test can miss some cases."
Reference: https://www.wbur.org/commonhealth/2020/07/30/shira-doron-covid-19-testing-types-accuracy
False positives are a problem with both tests, also. The FDA says the rate of false positives is expected to range from 20% to 70%, depending upon the specificity of the test and the percent of prevalence of COVID in the sample population. In practice, Most false-positive results are thought to be due to lab contamination or other problems with how the lab has performed the test. And that has been a very real problem.
The Mayo Clinic says:
The timing and type of antibody test affects accuracy. If you have testing too early in the course of infection, when the immune response is still building up in your body, the test may not detect antibodies. So antibody testing is not recommended until at least 14 days after the onset of symptoms. The U.S. Food and Drug Administration (FDA) authorized and verified certain antibody tests, but tests with questionable accuracy are still on the market.
MIT says about COVID-19 Testing accuracy: (June 2020)
If the specimen collection is not done perfectly, or if a patient is in an early stage of infection or already partially recovered from the illness, their nasal-swab sample might not contain enough viral material to come back positive. There are many stories about patients who tested negative soon after their symptoms began, only to test positive on a test done later. One case study describes a 34-year-old man who tested negative four times before finally testing positive five days after being admitted to a hospital.
The non-specific PCR test was rushed through with an emergency procedure and was never properly tested for non-research use. The creator of the test warned that this test was intended for research and not for diagnostic purposes. The PCR test works with cycles of amplification of genetic material, a piece of genome is amplified each time. Any contamination (such as other viruses, debris from old virus genomes) can possibly result in false positives.
The test does not tell you how many viruses are present in the sample, called the viral load, which real viral infection. If other words, just because someone tests positive, this does not mean that that person is actually clinically infected, is ill or is going to become ill.
A May 2020 study published in the Annals of Internal Medicine found getting tested the day a person is actually infected with coronavirus will likely yield a 100 percent false-negative rate; by day 8 after becoming infected, however, that rate drops to just 20 percent. Their conclusion was if you wait until the onset of coronavirus symptoms the odds of having an accurate test result increase dramatically.
The time it takes to process these tests can vary. You can visit your state or local health department's website to look for the latest local information on testing. If you hstate or localave symptoms of COVID-19 and want to get tested, call your healthcare provider first.
Ways to save money AND help the environment:
Eat healthier AND save money: Instant Pot Duo Crisp 11-in-1 Air Fryer and Electric Pressure Cooker Combo with Multicooker Lids that Fries, Steams, Slow Cooks, Sautés, Dehydrates
Save water AND money with this showerhead adapter, it lets the water flow until the water is hot, then shuts off water flow until you restart it, ShowerStart TSV Hot Water Standby Adapter
Protect your health with these:
Mattress Dust mite-Bedbug protector, 100% Waterproof, Hypoallergenic, Zippered
Handheld Allergen Vacuum Cleaner with UV Sanitizing and Heating for Allergies and Pet, Kills Mite, Virus, Molds, True HEPA with Powerful Suction removes Hair, Dander, Pollen, Dust,
Immune Support Supplement with Quercetin, Vitamin C, Zinc, Vitamin D3
GermGuardian Air Purifier with UV-C Light and HEPA 13 Filter, Removes 99.97% of Pollutants
5 Stage Air Purifier, Features Ultraviolet Light (UVC), H13 True Hepa, Carbon, PCO, Smart Wifi, Auto Mode, Quiet, Removes 99.97% of Particles, Smoke, Mold, Pet Dander, Dust, Odors
Interesting Reads:
THE PREPPER'S CANNING & PRESERVING BIBLE: [13 in 1] Your Path to Food Self-Sufficiency. Canning, Dehydrating, Fermenting, Pickling & More, Plus The Food Preservation Calendar for a Sustainable Pantry
The Backyard Homestead: Produce all the food you need on just a quarter acre! Paperback
The Citizens' Guide to Geologic Hazards: A Guide to Understanding Geologic Hazards Including Asbestos, Radon, Swelling Soils, Earthquakes, Volcanoes
The Uninhabitable Earth: Life After Warming
Book: The Sixth Extinction: An Unnatural History Paperback